Qualifying for Surgery
The criteria for weight loss surgery have recently been widened to reflect the high level of safety & effectiveness. Current eligibility criteria are:
The criteria for weight loss surgery have recently been widened to reflect the high level of safety & effectiveness. Current eligibility criteria are:

At Auckland Bariatric Surgery we understand that these surgeries represent a significant financial investment. We endeavour to have transparent costings and to minimise these where possible. All prices are GST inclusive.
As part of our kaupapa of patient centred care, we have made some changes to our pricing where you, the patient, can make choices for yourself.
The first was offering the choice of one night or two in hospital, and the most recent one is piloting two different options in the "package" of care after the surgery.
There is no difference in the preoperative journey - the same education, assessment and preparation is required, but after the surgery there is now a choice:
Streamline package - 2 years of ongoing support and education from our team
Extended package - 5 years of ongoing support and education from our team
This means there are a range of options available, which start from $19,200 for the one anastomosis 'mini' gastric bypass (OAGB). More details of what are included in each package can be found in our information pack, which is available by clicking on the yellow button at the bottom of this page.
A snapshot of the differences in the post operative pathways for the OAGB is outlined in the table below.
| Feature | Streamline Pathway | Extended Care Pathway |
|---|---|---|
| Overview | A simplified, lower-cost option including multidisciplinary care with fewer appointments and a more independent approach to care. | A comprehensive support package with additional consultations, multidisciplinary care, and structured follow-up. |
| Total Package Cost | from $19,200 | from $22,300 |
| Dietitian Support | 2 preoperative appointments 1 year post operative support (3 appointments) |
2 preoperative appointments 5 year post operative support (7 appointments) |
| Psychological Support | 1 preoperative assessment 1 post operative consultation. Further post operative support available on request (additional fees apply) |
1 preoperative assessment 2 year post operative support (5 appointments) |
| Post Operative Surgical Follow up | 2 year post operative support (5 appointments) | 5 year post operative support (10 appointments) |
Preoperative Costs
Initial Surgeon Consultation: $284
Preoperative Assessments: $977
Pre-surgery Very Low-Calorie Diet (VLCD): $200 - $500 dependent on time frame required.
Operative/Postoperative Costs
Mini (One Anastomosis) Gastric Bypass: from $19,200
Sleeve Gastrectomy: from $21,650
Roux-en-Y Gastric Bypass: from $21,616
Inclusive of postoperative follow-up package for our STREAMLINE option:
2 year Surgeon/nurse follow-up (5 appointments)
1 year dietitian support (3 appointments)
6 month psychologist support (1 appointment plus fee for service options)
Revisional Bariatric Surgery
Price estimates are for uncomplicated surgery. Special circumstances and additional procedures may result in additional charges. These prices may be subject to change.
There are other costs associated with having bariatric surgery to be considered.
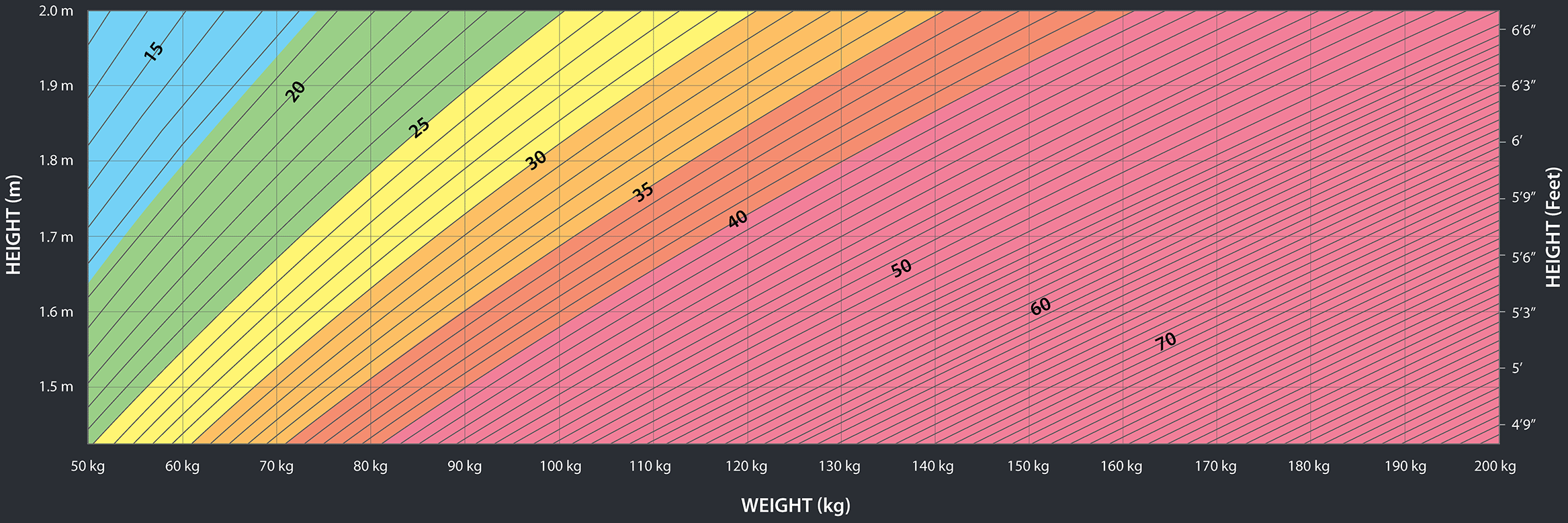
The core criteria are:
Please note that these criteria have been been extended, as reflection of the high level of both safety and efficacy that are achieved with modern keyhole techniques.
At Auckland Bariatric Surgery we endeavour to have transparent costings and to minimise these where possible. All prices are GST inclusive and start from $19,200 for the 'mini' one anastomosis gastric bypass under our Streamline option for post operative care. Please download our Information pack for more information or contact us directly on reception@bariatricsurgery.co.nz.
For patients who have had revisional surgery the process is slightly different and as such there may be additional procedural fees above the fixed price laid out in the patient information pack. Please contact us directly on reception@bariatricsurgery.co.nz for more detailed information.
It usually takes a minimum of 4-8 weeks to get surgery, from the time of the first appointment with me. Bariatric surgery is very safe but it is important to get prepared properly.
The actual kilogram amount will vary depending on what weight you started at. Generally at 1 year out from the surgery, you will have lost 70-80% of the weight above your "ideal" weight, which is set at a BMI of 25.
For example, a 170cm (5' 7") tall woman who weighs 130 kg has a BMI of 45. I would expect her to lose around 40-46 kg by 12 months.
There is no one, "best" operation. That is why I offer three options! The operations have different risk and benefit profiles; the choice of operation needs to be tailored with each patient individually. Generally speaking, I prefer the gastric bypasses (one anastomosis, or "mini" and the Roux-en-Y) but some patients can't have a bypass and so for them the sleeve gastrectomy is the best option.
The most important decision is actually realising that surgery is needed in the first place.
Some insurers may contribute to the cost of surgery and consultations. Please check this with your insurance company. We are happy to write to your insurer on your behalf.
Some of our patients who are contributing to a Kiwisaver scheme have been eligible for a one off withdrawal to cover the costs of this type of health-related surgery. Contact your provider for more information.
Yes we can. Please just email us with your request and include your full name and address.

Dr Benjamin Wheeler, Bariatric Surgeon
BHB MBChB FRACS

Anna McPhail, Registered Nurse
BNursing PGCertTM

Juliet Herlihy, Practice Manager
B.Com (Marketing & Management), B. Ph.Ed, Grad.Dip Teaching (Secondary)

Deirdre Nielson, Dietitian
NZRD, MHSC (Nutrition & Dietetics)

Sarah Mavor, Dietitian

Shona Collins, Dietitian

Kalpana Govind, Clinical Psychologist

Waheeda Goga, Clinical Psychologist
MA Soc Sci Clinical Psychology
If you have previously had weight loss surgery, or have further questions, please use the webform at the bottom of the page.
Visit our blog or Facebook page to read more of our articles.
Published on Friday, 30th January 2026
ok ok its late January but IMO this is still acceptable any time up until Waitangi weekend.
Every year since about 2021 I have thought at New Year's, maybe this year won't be quite the dumpster fire that last year was...not a great start so far, between the tragic landslide at Mount Maunganui and the flooding up North. Our hearts and minds go out to everyone who has been affected.
This is a time of goals and goal setting; I am going to use this as a kicking off point to look at goal setting from some different perspectives. The goals of a bariatric journey are the direction in which you are travelling, and the habits you form are what gets you there. (well technically the surgery gets you there, but the habits keep you there...the metaphor is getting wrecked now).
This is usually the period where the New Year's resolutions are falling apart a bit. Here is the first "habit" - abandon black and white thinking. A well constructed goal will help with this but think about success in shades of grey. My goal was to post here every week this year. Not a well designed goal, so I haven't achieved that. Posting today does give me a bit of a measure of success.
I'm going to post more about what makes for good goals but in general they should be SMART: specific, measurable, achievable, relevant and time-bound.
So my goal of posting every week is specific and measurable, maybe not achievable though as it turns out...definitely relevant and the time bound will be by the end of the year. So to be kind to myself, how many weeks of the year can I achieve this? A better goal might be, post every week, for at least 40 weeks of the year. Then there is a little bit of wiggle room.
Next week: some common goals my patients have and how to re-frame them to be better.
Hei te wā. Ben
Visit our blog or Facebook page to read more of our articles.